Featured post
Chapter 14: BREATHING AND EXCHANGE OF GASES NEET NOTES
- Get link
- X
- Other Apps
- Breathing is the process of exchanging oxygen (O2) from the atmosphere with carbon dioxide (CO2) produced by the cells.
- Oxygen is utilized by organisms to break down simple molecules like glucose, amino acids, and fatty acids to derive energy for various activities.
- Carbon dioxide, a harmful byproduct of these catabolic reactions, needs to be released from the cells.
- The respiratory organs are responsible for the exchange of gases during breathing.
- When we breathe, our chest moves up and down. This movement is a result of the mechanism of breathing.
- The primary respiratory organs are the lungs, which are located in the chest cavity.
- Breathing involves two main phases: inhalation and exhalation.
- During inhalation, the diaphragm and intercostal muscles contract, expanding the chest cavity and creating a vacuum. This leads to the intake of air into the lungs.
- Oxygen from the inhaled air diffuses into the bloodstream through tiny air sacs called alveoli in the lungs.
- Carbon dioxide, produced as a waste product in cells, is carried by the bloodstream back to the lungs.
- During exhalation, the diaphragm and intercostal muscles relax, causing the chest cavity to decrease in size. This forces air, along with carbon dioxide, out of the lungs and into the atmosphere.
- The exchange of gases between the lungs and the bloodstream occurs through a process called diffusion.
- Breathing is regulated by the respiratory center in the brain, which monitors the levels of oxygen and carbon dioxide in the body.
- Factors such as physical activity, altitude, and certain medical conditions can influence the rate and depth of breathing.
- Breathing is essential for maintaining the supply of oxygen to cells and removing carbon dioxide, ensuring the proper functioning of the body's metabolic processes.
14.1 RESPIRATORY ORGANS
- Lower invertebrates such as sponges, coelenterates, and flatworms exchange oxygen (O2) and carbon dioxide (CO2) through simple diffusion across their entire body surface.
- Earthworms rely on their moist cuticle for gas exchange, absorbing oxygen from the environment and releasing carbon dioxide.
- Insects have a network of tubes called tracheal tubes that transport atmospheric air directly to their body tissues for gas exchange.
- Aquatic arthropods and mollusks utilize specialized vascularized structures called gills for respiration, extracting oxygen from water and releasing carbon dioxide.
- Terrestrial organisms, including many arthropods and mollusks, as well as all vertebrates, use lungs for gas exchange. Lungs are vascularized sacs that facilitate the exchange of oxygen and carbon dioxide between the air and the bloodstream.
- Fishes respire through gills, which are highly vascularized structures that extract oxygen from water as it passes over them.
- Amphibians, such as frogs, respire through both lungs and their moist skin, known as cutaneous respiration. They can extract oxygen from the surrounding water or air.
- Reptiles, birds, and mammals respire exclusively through lungs. Lungs provide a larger surface area for efficient gas exchange in terrestrial environments.
- Cutaneous respiration, where gases are exchanged through the skin, is limited to certain amphibians and some other organisms living in moist environments.
- The exchange of gases in gills, lungs, or skin occurs through diffusion, where oxygen moves from areas of high concentration to areas of low concentration.
- The respiratory organs and mechanisms of breathing are adapted to the specific needs and environments of different organisms, allowing them to efficiently obtain oxygen and remove carbon dioxide.
14.1.1 Human Respiratory System
- The respiratory system begins with a pair of external nostrils located above the upper lips, which lead to the nasal chamber through the nasal passage.
- The nasal chamber opens into the pharynx, a common passage for both food and air.
- The pharynx opens into the larynx region, which contains the larynx, a cartilaginous box involved in sound production.
- The glottis, located in the larynx, can be covered by the epiglottis, a thin elastic cartilaginous flap, during swallowing to prevent the entry of food into the larynx.
- The trachea, a straight tube, extends from the larynx to the mid-thoracic cavity. It is commonly known as the windpipe.
- The trachea divides into the right and left primary bronchi at the level of the 5th thoracic vertebra.
- The bronchi further divide into secondary and tertiary bronchi, and then into bronchioles, which eventually lead to terminal bronchioles.
- The trachea, primary, secondary, and tertiary bronchi, as well as initial bronchioles, are supported by incomplete cartilaginous rings.
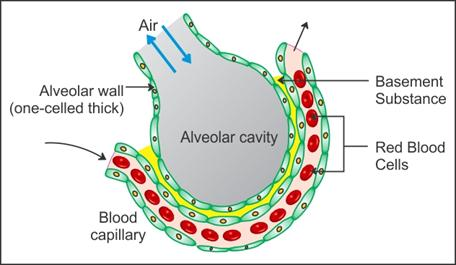
- Each terminal bronchiole gives rise to alveoli, which are thin, irregular-walled, and vascularized bag-like structures.
- The lungs consist of a branching network of bronchi, bronchioles, and alveoli.
- The lungs are covered by a double-layered pleura, with pleural fluid between them, reducing friction on the lung surface.
- The conducting part of the respiratory system, from the external nostrils to the terminal bronchioles, transports atmospheric air, humidifies it, clears foreign particles, and brings it to body temperature.
- The respiratory or exchange part of the respiratory system includes the alveoli and their ducts, where the actual diffusion of oxygen (O2) and carbon dioxide (CO2) occurs between the blood and atmospheric air.
- The thoracic chamber, formed by the vertebral column, sternum, ribs, and diaphragm, houses the lungs and is anatomically an air-tight chamber.
- Changes in the volume of the thoracic cavity affect the volume of the lung (pulmonary cavity), which is essential for breathing.
- Respiration involves several steps: breathing or pulmonary ventilation, diffusion of gases across the alveolar membrane, transport of gases by the blood, diffusion of oxygen and carbon dioxide between the blood and tissues, and the utilization of oxygen by cells for catabolic reactions and the release of carbon dioxide.
14.2 MECHANISM OF BREATHING
- Breathing consists of two stages: inspiration and expiration.
- Inspiration is the process of drawing atmospheric air into the lungs, while expiration is the release of alveolar air out of the lungs.
- The movement of air into and out of the lungs is driven by creating a pressure gradient between the lungs and the atmosphere.
- During inspiration, the intra-pulmonary pressure (pressure within the lungs) becomes lower than the atmospheric pressure, resulting in a negative pressure in the lungs.
- The diaphragm, a dome-shaped muscle, contracts during inspiration, increasing the volume of the thoracic chamber in the antero-posterior axis.
- The external intercostal muscles, located between the ribs, lift up the ribs and sternum, further increasing the volume of the thoracic chamber in the dorso-ventral axis.
- The overall increase in thoracic volume leads to a corresponding increase in pulmonary volume, creating a lower intra-pulmonary pressure.
- The decrease in intra-pulmonary pressure compared to atmospheric pressure causes air from outside to move into the lungs, resulting in inspiration.
- During expiration, the diaphragm and intercostal muscles relax, returning to their normal positions and reducing the thoracic volume.
- The reduction in thoracic volume leads to an increase in intra-pulmonary pressure, slightly above atmospheric pressure.
- The increase in intra-pulmonary pressure during expiration causes the expulsion of air from the lungs.
- Additional muscles in the abdomen can assist in increasing the strength of inspiration and expiration if needed.
- On average, a healthy human breathes 12-16 times per minute.
- The volume of air involved in breathing movements can be measured using a spirometer, which helps in the clinical assessment of pulmonary functions.
14.2.1 Respiratory Volumes and Capacities
Tidal Volume (TV): The volume of air inspired or expired during normal respiration is approximately 500 mL. A healthy individual can inspire or expire around 6000 to 8000 mL of air per minute.
Inspiratory Reserve Volume (IRV): The additional volume of air that a person can inspire by a forcible inspiration average between 2500 mL to 3000 mL.
Expiratory Reserve Volume (ERV): The additional volume of air that a person can expire by a forcible expiration average between 1000 mL to 1100 mL.
Residual Volume (RV): The volume of air that remains in the lungs even after a forcible expiration average between 1100 mL to 1200 mL.
Inspiratory Capacity (IC): The total volume of air that a person can inspire after a normal expiration. It includes the tidal volume and inspiratory reserve volume (TV + IRV).
Expiratory Capacity (EC): The total volume of air that a person can expire after a normal inspiration. It includes the tidal volume and expiratory reserve volume (TV + ERV).
Functional Residual Capacity (FRC): The volume of air that remains in the lungs after a normal expiration. It includes the expiratory reserve volume and residual volume (ERV + RV).
Vital Capacity (VC): The maximum volume of air that a person can breathe in after a forced expiration. It includes the expiratory reserve volume, tidal volume, and inspiratory reserve volume.
Total Lung Capacity (TLC): The total volume of air accommodated in the lungs at the end of forced inspiration. It includes the residual volume, expiratory reserve volume, tidal volume, and inspiratory reserve volume, or it can be calculated as the sum of vital capacity and residual volume.
14.3 EXCHANGE OF GASES
- Alveoli are the primary sites of gas exchange, where oxygen (O2) and carbon dioxide (CO2) are exchanged between the air and the blood.
- Exchange of gases also occurs between the blood and the tissues.
- The exchange of gases in these sites occurs through simple diffusion based on pressure or concentration gradients.
- Partial pressure refers to the pressure contributed by an individual gas in a mixture of gases. The partial pressure of oxygen is represented as pO2, and the partial pressure of carbon dioxide is represented as pCO2.
- There is a concentration gradient for oxygen from the alveoli to the blood and from the blood to the tissues, as indicated by the data in Table 14.1 and Figure 14.3.
- Conversely, there is a concentration gradient for carbon dioxide in the opposite direction, from the tissues to the blood and from the blood to the alveoli.
- The solubility of CO2 is 20-25 times higher than that of O2. This means that a greater amount of CO2 can diffuse through the diffusion membrane per unit difference in partial pressure compared to O2.
- The diffusion membrane involved in gas exchange is composed of three major layers: the thin squamous epithelium of the alveoli, the endothelium of alveolar capillaries, and the basement substance between them.
- The total thickness of the diffusion membrane is much less than a millimeter, allowing efficient diffusion of gases.
- All the factors in our body, including the concentration gradients, solubility of gases, and the thinness of the diffusion membrane, favor the diffusion of O2 from the alveoli to the tissues and the diffusion of CO2 from the tissues to the alveoli.
14.4 TRANSPORT OF GASES
- Blood serves as the medium of transport for oxygen (O2) and carbon dioxide (CO2) in the body.
- Approximately 97% of the oxygen is transported by red blood cells (RBCs) in the blood.
- The remaining 3% of oxygen is carried in a dissolved state through the plasma.
- Around 20-25% of carbon dioxide is transported by RBCs.
- The majority of carbon dioxide (70%) is transported as bicarbonate (HCO3-) ions in the plasma.
- About 7% of carbon dioxide is carried in a dissolved state through the plasma.
14.4.1 Transport of Oxygen
- Hemoglobin is a red-colored iron-containing pigment present in red blood cells (RBCs).
- Oxygen (O2) can bind with hemoglobin in a reversible manner to form oxyhemoglobin.
- Each hemoglobin molecule can carry a maximum of four molecules of oxygen.
- The binding of oxygen with hemoglobin is primarily influenced by the partial pressure of oxygen (pO2).
- Other factors such as partial pressure of carbon dioxide (pCO2), hydrogen ion concentration (pH), and temperature can also affect the binding of oxygen to hemoglobin.
- The oxygen dissociation curve, represented by a sigmoid curve, shows the percentage saturation of hemoglobin with oxygen plotted against pO2. It helps in studying the effect of factors like pCO2, pH, etc., on the binding of oxygen with hemoglobin.
- In the alveoli, where there is high pO2, low pCO2, lower H+ concentration, and lower temperature, the conditions are favorable for the formation of oxyhemoglobin.
- In the tissues, where there is low pO2, high pCO2, higher H+ concentration, and higher temperature, the conditions are favorable for the dissociation of oxygen from oxyhemoglobin.
- This indicates that oxygen binds to hemoglobin in the lungs and dissociates from it in the tissues, facilitating the delivery of oxygen to the tissues.
- Under normal physiological conditions, approximately 5 ml of oxygen can be delivered to the tissues by every 100 ml of oxygenated blood.
14.4.2 Transport of Carbon dioxide
- Carbon dioxide (CO2) is carried by hemoglobin as carbamino-hemoglobin, accounting for about 20-25% of CO2 transport.
- The binding of CO2 to hemoglobin is influenced by the partial pressure of CO2 (pCO2).
- When pCO2 is high and pO2 is low, as in the tissues, more binding of CO2 to hemoglobin occurs.
- When pCO2 is low and pO2 is high, as in the alveoli, dissociation of CO2 from carbamino-hemoglobin takes place, allowing CO2 bound to hemoglobin from the tissues to be delivered at the alveoli.
- Red blood cells (RBCs) contain a high concentration of the enzyme carbonic anhydrase, which facilitates the conversion of CO2 and water (H2O) into carbonic acid (H2CO3).
- The carbonic acid (H2CO3) formed further dissociates into bicarbonate ions (HCO3-) and hydrogen ions (H+).
- At the tissue site, where pCO2 is high, CO2 diffuses into the blood (RBCs and plasma) and forms bicarbonate and H+ ions.
- At the alveolar site, where pCO2 is low, the reaction proceeds in the opposite direction, leading to the formation of CO2 and water from bicarbonate and H+ ions.
- CO2 trapped as bicarbonate at the tissue level is transported to the alveoli and released as CO2.
- Approximately 4 ml of CO2 is delivered to the alveoli by every 100 ml of deoxygenated blood.
14.5 REGULATION OF RESPIRATION
- The respiratory rhythm in human beings is regulated by the neural system.
- The respiratory rhythm center, located in the medulla region of the brain, is responsible for regulating and maintaining the respiratory rhythm.
- The pneumotaxic center, located in the pons region of the brain, can modulate the functions of the respiratory rhythm center.
- The pneumotaxic center can reduce the duration of inspiration and, consequently, alter the respiratory rate.
- Adjacent to the rhythm center is a chemosensitive area that is highly sensitive to changes in carbon dioxide (CO2) and hydrogen ion concentration (H+).
- Increased levels of CO2 and H+ can activate the chemosensitive area, which then signals the rhythm center to make necessary adjustments in the respiratory process to eliminate these substances.
- Receptors associated with the aortic arch and carotid artery can also detect changes in CO2 and H+ concentration and send signals to the rhythm center for appropriate actions.
- Oxygen has a minimal role in the regulation of respiratory rhythm and is not a major factor in the control of respiration.
14.6 DISORDERS OF THE RESPIRATORY SYSTEM
- Asthma is a respiratory condition characterized by difficulty in breathing and wheezing. It is caused by inflammation of the bronchi and bronchioles.
- Emphysema is a chronic disorder where the alveolar walls in the lungs are damaged, leading to a decrease in the respiratory surface area.
- Cigarette smoking is one of the major causes of emphysema. Prolonged exposure to cigarette smoke can result in the destruction of alveolar walls and impairment of lung function.
- Occupational respiratory disorders can occur in certain industries where high levels of dust or particulate matter are produced. The body's defense mechanisms may not be able to cope with excessive dust exposure, leading to inflammation and fibrosis (proliferation of fibrous tissues) in the lungs.
- Workers in industries with high dust levels, such as grinding or stone-breaking, should wear protective masks to reduce their exposure and minimize the risk of developing occupational respiratory disorders.
Summary Mind Map
- Get link
- X
- Other Apps







Comments
Post a Comment